- La bithérapie anti-plaquettaire réduit les récidives ischémiques après un syndrome coronarien aigu ou la pose d’un stent coronaire, mais augmente le risque hémorragique
- Le choix de la durée du traitement doit être équilibré entre l’avantage de prévenir les événements ischémiques et le risque hémorragique
- La durée optimale de la bithérapie anti-plaquettaire après pose de stent n’est pas encore consensuelle
L’étude publiée par F Costa et al dans le Lancet décrit le calcul du score PRECISE-DAPT qui est un score de risque simple calculé sur cinq items, qui fournit un outil de prédiction du risque hémorragique à la sortie de l’hôpital. Avec une validation interne et externe robuste, les auteurs montrent que cet outil prédit le bénéfice clinique net de la bithérapie et peut ainsi constituer une aide à la prise de décision clinique concernant la durée de la bithérapie anti-plaquettaire.
Costa F et al. 2017. Lancet 389:1025.
Téléchargement (pour les abonnés seulement): PRECISE_DAPT_2017.pdf
Le calculateur est accessible en ligne : CALCULATEUR
Costa, F., D. van Klaveren, S. James, D. Heg, L. Raber, F. Feres, T. Pilgrim, M. K. Hong, H. S. Kim, A. Colombo, P. G. Steg, T. Zanchin, T. Palmerini, L. Wallentin, D. L. Bhatt, G. W. Stone, S. Windecker, E. W. Steyerberg, M. Valgimigli, and P.-D. S. Investigators. 2017.
Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials.
Lancet 2017. 389: 1025-1034. PubMed.
BACKGROUND: Dual antiplatelet therapy (DAPT) with aspirin plus a P2Y12 inhibitor prevents ischaemic events after coronary stenting, but increases bleeding. Guidelines support weighting bleeding risk before the selection of treatment duration, but no standardised tool exists for this purpose.
METHODS: A total of 14 963 patients treated with DAPT after coronary stenting-largely consisting of aspirin and clopidogrel and without indication to oral anticoagulation-were pooled at a single-patient level from eight multicentre randomised clinical trials with independent adjudication of events. Using Cox proportional hazards regression, we identified predictors of out-of-hospital Thrombosis in Myocardial Infarction (TIMI) major or minor bleeding stratified by trial, and developed a numerical bleeding risk score. The predictive performance of the novel score was assessed in the derivation cohort and validated in patients treated with percutaneous coronary intervention from the PLATelet inhibition and patient Outcomes (PLATO) trial (n=8595) and BernPCI registry (n=6172). The novel score was assessed within patients randomised to different DAPT durations (n=10 081) to identify the effect on bleeding and ischaemia of a long (12-24 months) or short (3-6 months) treatment in relation to baseline bleeding risk.
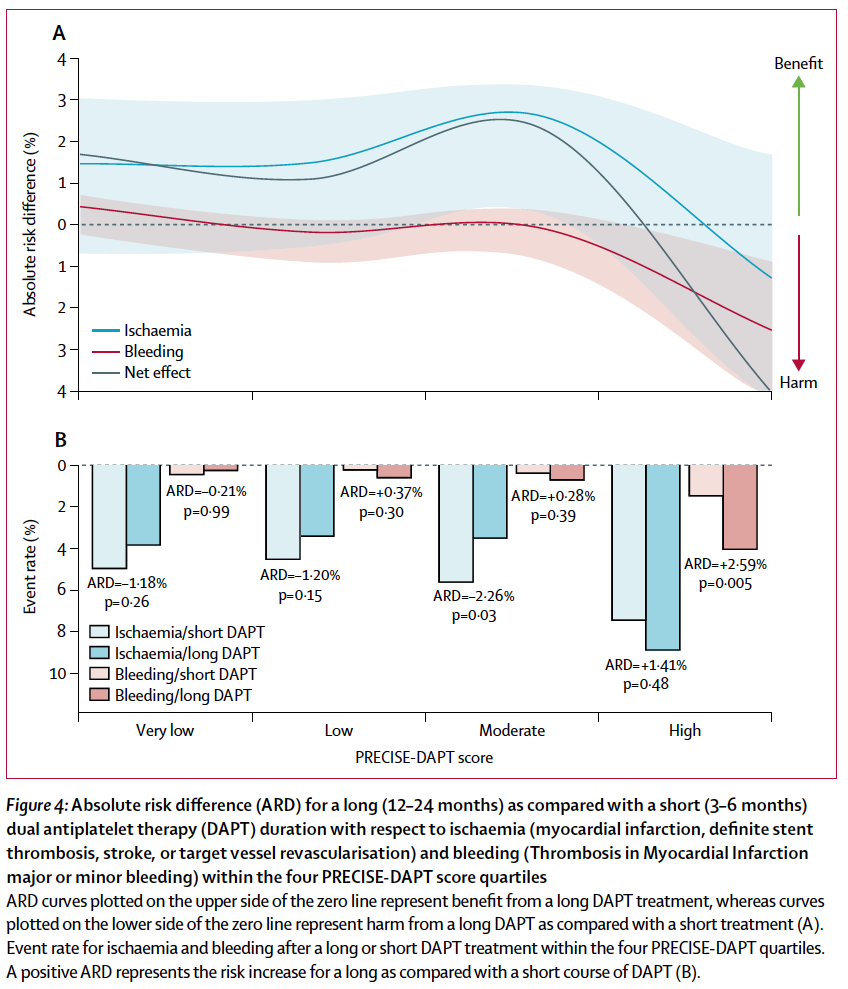
FINDINGS: The PRECISE-DAPT score (age, creatinine clearance, haemoglobin, white-blood-cell count, and previous spontaneous bleeding) showed a c-index for out-of-hospital TIMI major or minor bleeding of 0.73 (95% CI 0.61-0.85) in the derivation cohort, and 0.70 (0.65-0.74) in the PLATO trial validation cohort and 0.66 (0.61-0.71) in the BernPCI registry validation cohort. A longer DAPT duration significantly increased bleeding in patients at high risk (score >/=25), but not in those with lower risk profiles (pinteraction=0.007), and exerted a significant ischaemic benefit only in this latter group.
INTERPRETATION: The PRECISE-DAPT score is a simple five-item risk score, which provides a standardised tool for the prediction of out-of-hospital bleeding during DAPT. In the context of a comprehensive clinical evaluation process, this tool can support clinical decision making for treatment duration.