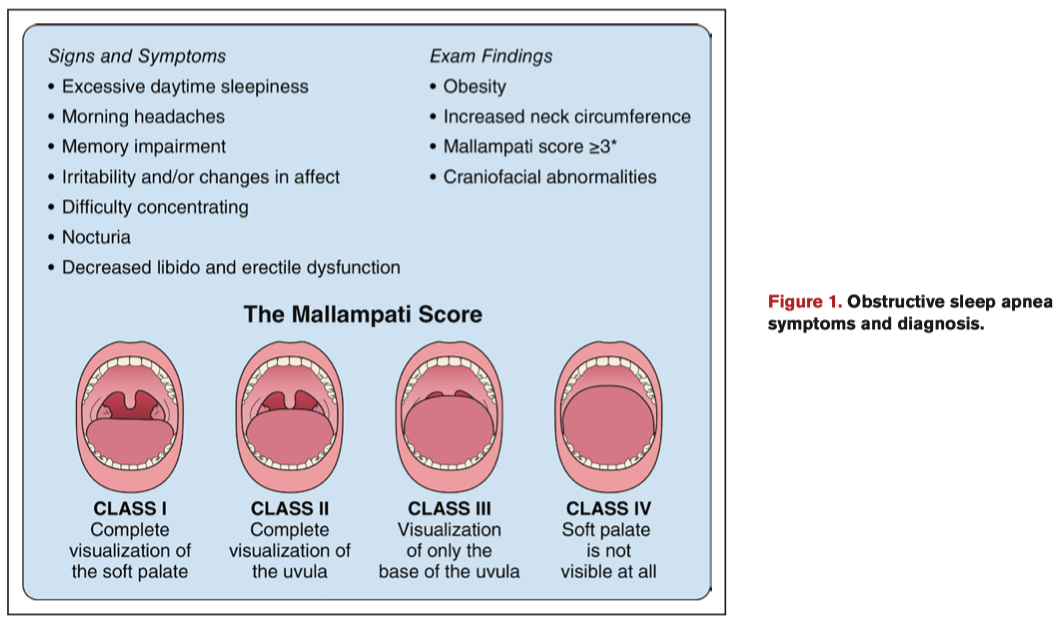
L’apnée obstructive du sommeil (AOS) est caractérisée par des événements obstructifs récurrents complets et partiels des voies aériennes supérieures, entraînant une hypoxémie intermittente, une fluctuation du tonus autonome et une fragmentation du sommeil. Environ 34 % des hommes et 17% des femmes d’âge moyen répondent aux critères diagnostiques de l’AOS. La prévalence de l’AOS est 40 à 80 % chez les patients souffrant d’hypertension, d’insuffisance cardiaque, de maladie coronarienne, d’hypertension pulmonaire, de fibrillation auriculaire et d’accident vasculaire cérébral. Malgré sa prévalence élevée chez les patients atteints de maladies cardiaques et la vulnérabilité des patients cardiaques aux facteurs de stress liés à l’AOS et aux conséquences cardiovasculaires indésirables, l’AOS est souvent sous-estimée et sous-traitée dans la prise en charge des patients cardiovasculaires.
L’AHA (American Heart Association) recommande désormais le dépistage et la prise en charge de l’AOS chez les patients cardiovasculaires comme détaillé dans l’article ci-dessous.
Obstructive Sleep Apnea and Cardiovascular Disease: A Scientific Statement From the American Heart Association
Yeghiazarians Y, Jneid H, Tietjens JR, Redline S, Brown DL, El-Sherif N, Mehra R, Bozkurt B, Ndumele CE, Somers VK
Circulation. 2021;143:00–00. DOI: 10.1161/CIR.0000000000000988
Obstructive sleep apnea (OSA) is characterized by recurrent complete and partial upper airway obstructive events, resulting in intermittent hypoxemia, autonomic fluctuation, and sleep fragmentation. Approximately 34% and 17% of middle-aged men and women, respectively, meet the diagnostic criteria for OSA. Sleep disturbances are common and underdiagnosed among middle-aged and older adults, and the prevalence varies by race/ethnicity, sex, and obesity status. OSA prevalence is as high as 40% to 80% in patients with hypertension, heart failure, coronary artery disease, pulmonary hypertension, atrial fibrillation, and stroke. Despite its high prevalence in patients with heart disease and the vulnerability of cardiac patients to OSA-related stressors and adverse cardiovascular outcomes, OSA is often underrecognized and undertreated in cardiovascular practice. We recommend screening for OSA in patients with resistant/poorly controlled hypertension, pulmonary hypertension, and recurrent atrial fibrillation after either cardioversion or ablation. In patients with New York Heart Association class II to IV heart failure and suspicion of sleep-disordered breathing or excessive daytime sleepiness, a formal sleep assessment is reasonable. In patients with tachy-brady syndrome or ventricular tachycardia or survivors of sudden cardiac death in whom sleep apnea is suspected after a comprehensive sleep assessment, evaluation for sleep apnea should be considered. After stroke, clinical equipoise exists with respect to screening and treatment. Patients with nocturnally occurring angina, myocardial infarction, arrhythmias, or appropriate shocks from implanted cardioverter-defibrillators may be especially likely to have comorbid sleep apnea. All patients with OSA should be considered for treatment, including behavioral modifications and weight loss as indicated. Continuous positive airway pressure should be offered to patients with severe OSA, whereas oral appliances can be considered for those with mild to moderate OSA or for continuous positive airway pressure-intolerant patients. Follow-up sleep testing should be performed to assess the effectiveness of treatment.