La perte de dents est souvent utilisée comme indicateur d’une mauvaise santé bucco-dentaire et a été associée aux maladies cardiovasculaires (MCV). Cependant, la perte de dents est une évaluation statique de la santé bucco-dentaire et représente le stade final des maladies bucco-dentaires non traitées, principalement la carie dentaire et la parodontite. La capacité masticatoire, telle qu’évaluée par le nombre d’unités masticatoires fonctionnelles (UFA), englobe non seulement l’histoire des maladies bucco-dentaires comme le nombre de dents manquantes, mais aussi une partie de la physiologie buccale, c’est-à-dire la capacité de mastication. Cet aspect multidimensionnel fait du nombre d’UFA une métrique plus inclusive que le nombre de dents manquantes.
Dans cette étude, le lien entre mastication et biomarqueurs cardiovasculaires a été testé. Il s’agit de la première étude communautaire examinant la relation entre une faible capacité masticatoire et les niveaux de biomarqueurs d’inflammation de bas grade, de lésion myocardique et de stress cardiomyocytaire.
Eirini Chatzopoulou , Hélène Rangé, Omar Deraz, Pierre Boutouyrie , Marie-Cécile Perier, Catherine Guibout, Frédérique Thomas, Muriel Andrieu , Karine Bailly, Benoît Vedie , Nicolas Danchin , Xavier Jouven, Philippe Bouchard, Jean-Philippe Empana
Poor Masticatory Capacity and Blood Biomarkers of Elevated Cardiovascular Disease Risk in the Community: The Paris Prospective Study III
Arteriosclerosis, Thrombosis, and Vascular Biology. 2021;DOI: 10.1161/ATVBAHA.121.316085. PubMed.
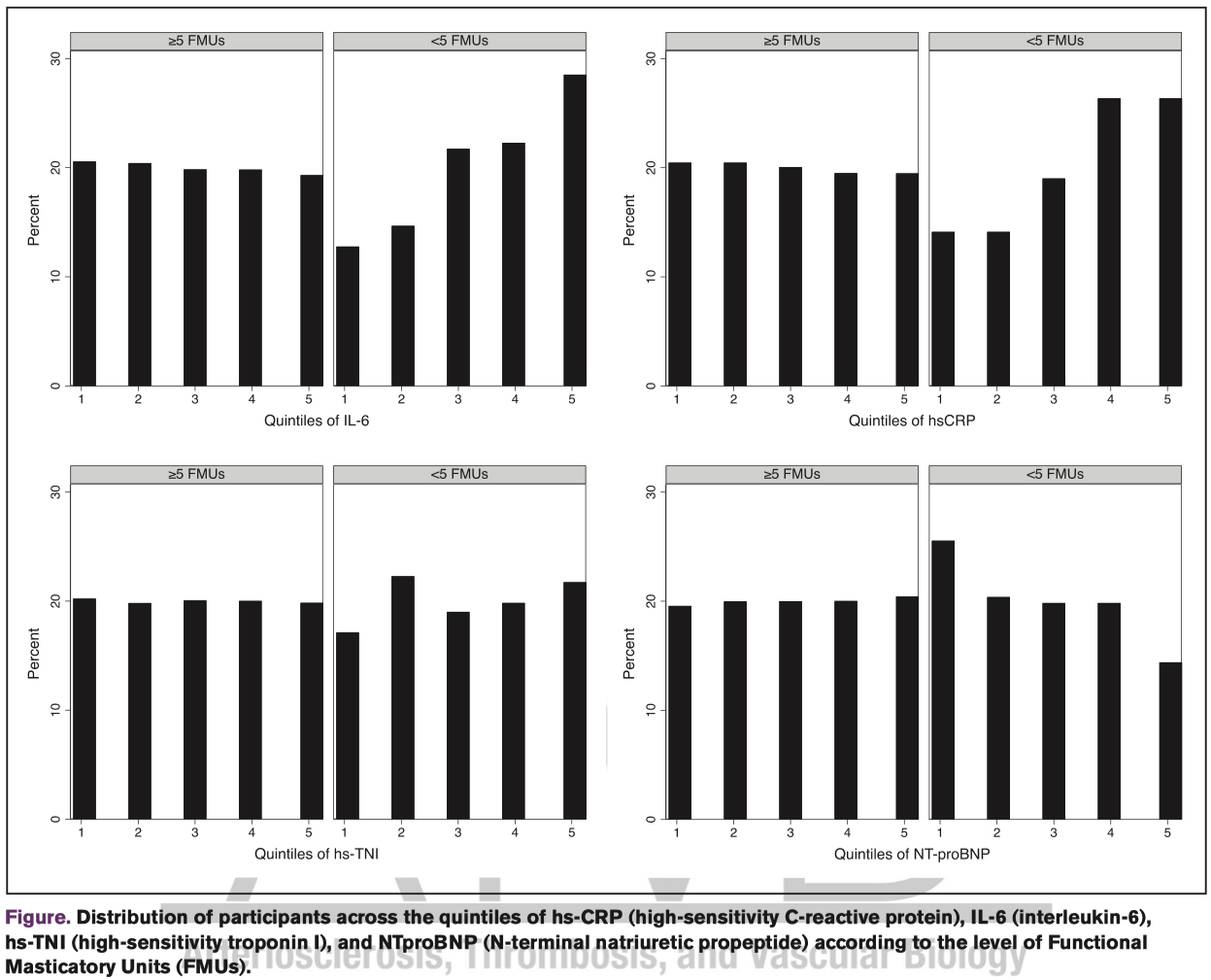
Objective: The mechanisms underlying the association between low number of masticatory units and cardiovascular disease remain unclear. Under a nutritional framework, we hypothesized that poor masticatory capacity could represent an early sign of elevated cardiovascular disease risk as evaluated by circulating markers of systemic inflammation and cardiomyocyte stress or damage. Approach and Results: In this cross-sectional analysis of the Paris Prospective Study III, a community-based observational study, 4837 adults aged 50 to 75 without cardiovascular disease history underwent a full-mouth clinical examination and plasma NTproBNP (N-terminal natriuretic propeptide), hs-CRP (high-sensitivity C-reactive protein), IL-6 (interleukin-6), hs-TNI (high-sensitivity troponin I) were measured using highly sensitive technics. Poor masticatory capacity was defined as <5 functional masticatory units, that is, pairs of opposing natural or prosthetically replaced posterior teeth. In linear regression analysis accounting for sociodemographic factors, cardiovascular disease risk factors, gingival inflammation, and body mass index, poor masticatory capacity was significantly associated with lower levels of NTproBNP (β=-0.11, P=0.045). The significant association between poor masticatory capacity and higher IL-6 in multivariable analysis was confounded by body mass index. There was no association between functional masticatory units and hs-TNI even in unadjusted analysis.
Conclusions: The present findings support a nutritional pathway whereby diet alterations and the resulting abdominal obesity associated with poor masticatory capacity may contribute to the higher level of IL-6 and to the lower level of NTproBNP, respectively.