Les mécanismes sous-jacents à la relation entre la maladie parodontale (MP) et les maladies coronariennes (MC) sont été insuffisamment explorés. Dans cet article publié dans le International Journal of Cardiology une étude d’association a été réalisée entre la perte de dents (sur la base de la déclaration des sujets) — un indicateur de MP — et la mesure de marqueur pronostiques chez 15 456 patients ayant une MC stable (essai STABILITY).
Vedin O, Hagstrom E, Ostlund O, Avezum A, Budaj A, Flather MD, Harrington RA, Koenig W, Soffer J, Siegbahn A, Steg PG, Stewart RAH, Wallentin L, White HD, Held C, Investigators (2017).
Associations between tooth loss and prognostic biomarkers and the risk for cardiovascular events in patients with stable coronary heart disease
Int J Cardiol. 2017. Sept. PubMed.
BACKGROUND: Underlying mechanisms behind the hypothesized relationship between periodontal disease (PD) and coronary heart disease (CHD) have been insufficiently explored. We evaluated associations between self-reported tooth loss- a marker of PD- and prognostic biomarkers in 15,456 (97%) patients with stable CHD in the global STABILITY trial.
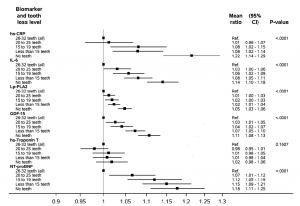
METHODS AND RESULTS: Baseline blood samples were obtained and patients reported their number of teeth according to the following tooth loss levels: « 26-32 (All) » [lowest level], « 20-25 », « 15-19 », « 1-14 », and « No Teeth » [highest level]. Linear and Cox regression models assessed associations between tooth loss levels and biomarker levels, and the relationship between tooth loss levels and outcomes, respectively. After multivariable adjustment, the relative biomarker increase between the highest and the lowest tooth loss level was: high-sensitivity C-reactive protein 1.21 (95% confidence interval, 1.14-1.29), interleukin 6 1.14 (1.10-1.18), lipoprotein-associated phospholipase A2 activity 1.05 (1.03-1.06), growth differentiation factor 15 1.11 (1.08-1.14), and N-terminal pro-B-type natriuretic peptide (NT-proBNP) 1.18 (1.11-1.25). No association was detected for high-sensitivity troponin T 1.02 (0.98-1.05). Some attenuation of the relationship between tooth loss and outcomes resulted from the addition of biomarkers to the multivariable analysis, of which NT-proBNP had the biggest impact.
CONCLUSIONS: A graded and independent association between tooth loss and several prognostic biomarkers was observed, suggesting that tooth loss and its underlying mechanisms may be involved in multiple pathophysiological pathways also implicated in the development and prognosis of CHD. The association between tooth loss and cardiovascular death and stroke persisted despite comprehensive adjustment including prognostic biomarkers.
CLINICAL TRIAL REGISTRATION: www.clinicaltrials.gov; NCT00799903.